Treatment Strategies for Shoulder Pain

In the first of this two-part series, we'll review why shoulder injuries are so complex to treat, and the evidence-base around using Photobiomodulation (laser therapy) to manage shoulder pain.
Shoulder pain is reported to be the third most prevalent orthopedic condition.1 Due to the complexity of the shoulder girdle, it is usually a problem that requires some level of professional intervention to restore function. Clinics can impact new patient traffic and overall revenue by creating specialized programs to address common shoulder conditions like chronic impingement, thrower’s shoulder, cuff pathology, and frozen shoulder.
Shoulder pain is unique because:
- It's Complex - The shoulder is the most mobile joint in the body.2 It requires multiple muscles and joints to work in harmony to allow normal function. Most patients presenting with shoulder pain have problem lists that require skilled intervention. Restoring glenohumeral rhythm is not an intuitive process for most patients and usually requires treatment components that cannot be addressed independently. These problems rarely fix themselves
- It Impacts Daily Function - Patients use their arms a lot. Having a painful shoulder can impact everything from sleeping to any activity that requires overhead motion. Shoulder pain is a commonly reported reason for having to miss work.1 Abnormal mechanics tend to worsen with time which frustrates most patients. This makes them a highly motivated patient population and places a premium on having treatment options that impact pain quickly, as it is paramount to improving shoulder function.
- It Takes Time - Shoulder problems often require longer plans of care due to a variety of factors that include: poor blood flow to tendinous structures, time required to build strength of the cuff musculature, time required to re-educate scapular muscles, and the challenges restoring motion at the glenohumeral and scapulothoracic complexes. These extended plans of care are highly desirable for most clinics but, if not managed well, can lead to higher rates of patient self-discharge.
- Its Prognosis - Several studies have reported that only 50% of patients presenting with shoulder pain achieve complete recovery after six months and only 60% after 12 months.3 Given the challenges these patients represent, plans of care need to be optimized and evidence-based whenever possible.
There is growing support for the use of passive modalities to help impact pain and clear the way for more active therapies.4 Passive modalities, such as laser therapy and extracorporeal shock wave therapy, combined with exercise have outperformed placebo devices and standard plans of care when treating conditions like frozen shoulder, cuff tendinopathy, calcification and impingement.5,6, 7 Laser therapy has actually been shown to be as effective as cortisone injection when addressing pain associated with shoulder impingement.8
A multimodal approach to managing shoulder conditions
Energy modalities are becoming more popular in the physical therapy, osteopath, chiropractic, and athletic training fields as research continues to support the benefit they provide when added to treatment protocols. The complexity of shoulder pain necessitates a multimodal approach to care, and incorporating modalities such as photobiomodulation therapy (PBMT), also known as laser therapy, and extracorporeal shock wave therapy, can help optimize patient outcomes.
The role of Photobiomodulation in relieving pain and improving mobility.
PBMT can result in beneficial therapeutic outcomes such as the alleviation of pain, increased blood flow, muscle relaxation, and relief from joint stiffness.9-11 Relieving pain and increasing muscle relaxation allows patients suffering from shoulder conditions to get more out of their therapy program which can lead to improved outcomes and an accelerated recovery.
PBMT is a form of light therapy based on the photochemical process called photobiomodulation (PBM). In photobiomodulation therapy, a light source is placed near or in contact with the skin; the light energy penetrates the skin, reaching the mitochondria of damaged or diseased tissue, leading to photobiomodulation.

Physiological effects of PBM12 include:
- Analgesic - Long lasting pain relief by having a direct influence on nocioceptive activation
- A significant reduction in inflammatory markers and neurotransmitters
- Increased synthesis of ATP
- Impacts the biochemical pathways involved in tissue repair
- Increased microcirculation
A conservative first-line treatment for shoulder pain
PBMT provides a drug-free, surgery-free, non-invasive pain treatment alternative that many patients with shoulder pain are searching for.
Research supports the use of laser therapy for shoulder pain
- Elsodany and colleagues demonstrated that laser therapy combined with exercise therapy is more effective at improving pain and function in patients with rotator cuff tendinopathy when compared to sham laser and exercise.13
- Kelle and Kozanoglu compared laser therapy to corticosteroid injection in patients with shoulder impingement and concluded that both treatments were more effective than sham laser in improving patient pain.8
- The Cochrane Review, Electrotherapy modalities for rotator cuff disease, concludes that laser therapy when compared to placebo may offer short-term benefits to patients with rotator cuff disease.29
- A review by Haslerud et al. reported that laser therapy, whether used alone or in conjunction with other physiotherapy treatments, can provide shoulder tendinopathy patients clinically significant pain relief.14
- A recent meta-analysis of clinical trials using laser therapy to treat musculoskeletal conditions demonstrated that laser therapy had the greatest functional impact on the shoulder (and knee) compared to other anatomical locations treated.15
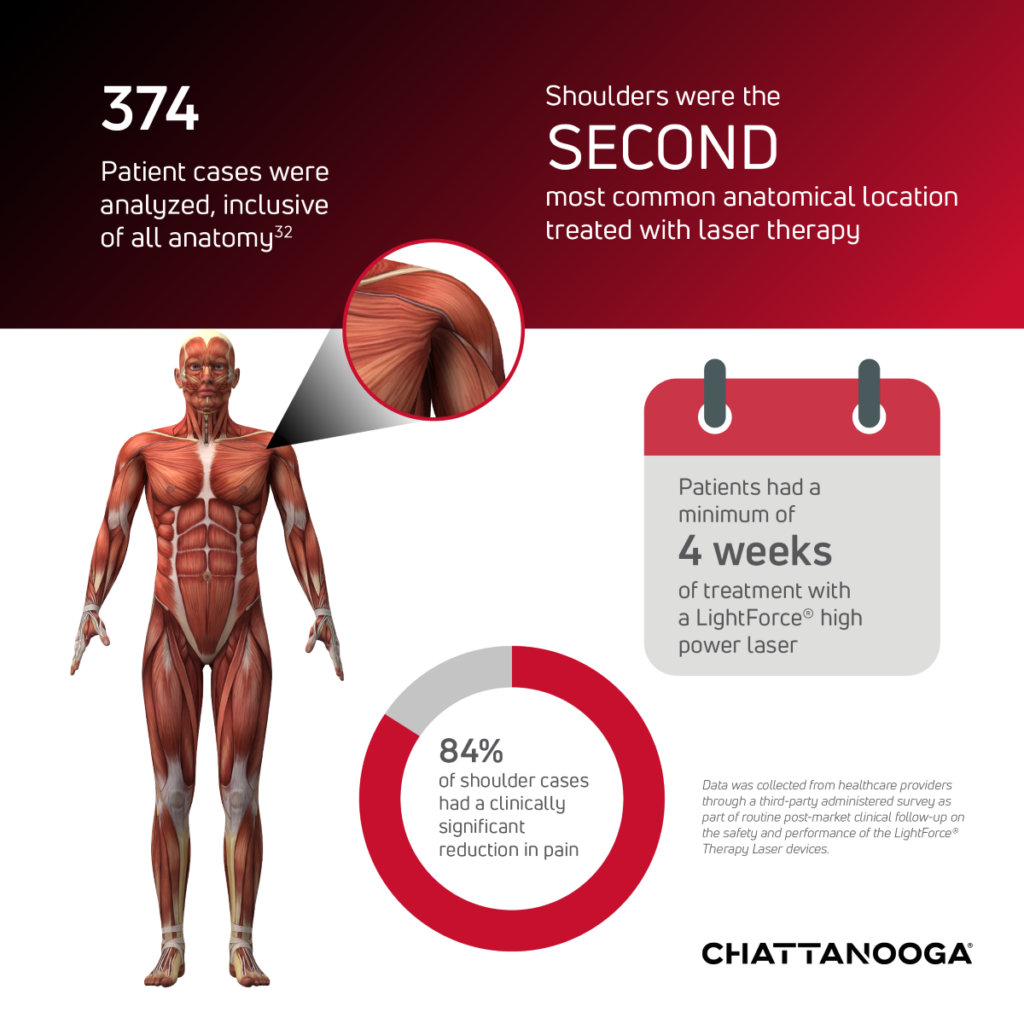
Use of Lightforce laser therapy to reduce pain
ESWT (Extracorporeal Shockwave Therapy)
ESWT (Extracorporeal Shockwave Therapy), which encompasses both Radial Shockwave (RSW) and Focus Shockwave (FSW) therapy, is a non-invasive treatment option that has support in the literature for helping address muscle aches and pains associated with shoulder dysfunction.16 During treatment with ESWT, high-energy sound waves are transmitted into the tissue propagating radially and creating a therapeutic effect on the impacted areas.17
How does ESWT help tissue?
High energy waves, called shockwaves, which can be created via different mechanisms, create a phenomenon called mechanotransduction. Simply put, it is the process of imparting brief, physical deformation to cells that leads to biochemical changes. These changes have the potential to
positively impact pain and tissue repair.18
In some instances, the negative pressure created during the tensile phase of a shockwave creates cavitation bubbles within cells.19 If intense enough, it can lead to disruption of damaged cells which is why ESWT can be classified as a proinflammatory modality. Disruption of cells can lead to cell death (apoptosis) which triggers a low-level inflammatory response that benefits the process of removal and replacement of damaged tissue. This is another way that RSW therapy can uniquely assist in treating chronic soft tissue problems.
In Part 2 we'll take a closer look at rotator cuff tendinopathy, including Rotator Cuff Calcification and the studies that support the use of shockwave therapy in the treatment of calcific tendonitis.
Request a demonstration of a Chattanooga Shockwave Therapy or Lightforce Therapy Laser HERE.
References:
- Hodgetts, C, Walker, B. Epidemiology, common diagnoses, treatments and prognosis of shoulder pain: A narrative review. Int J Osteopath Med. 2021; 42: 11-19.
- Chang LR, Anand P, Varacallo MA. Anatomy, Shoulder and Upper Limb, Glenohumeral Joint. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537018/
- van Doorn PF, de Schepper EIT, Rozendaal RM, et al. The incidence and management of shoulder complaints in general practice: a retrospective cohort study. Fam Pract. 2021;38(5):582-588.
- Dowell D, Ragan KR, Jones CM, et al.. CDC Clinical Practice Guideline for Prescribing Opioids for Pain — United States, 2022. MMWR Recomm Rep. 2022 Nov 4;71(3):1-95.
- Page MJ, Green S, Kramer S, Johnston RV, McBain B, Buchbinder R. Electrotherapy modalities for adhesive capsulitis (frozen shoulder). Cochrane Database Syst Rev. 2014;2014(10):CD011324. Published 2014 Oct 1.
- Elsodany AM, Alayat MSM, Ali MME, Khaprani HM. Long-Term Effect of Pulsed Nd:YAG Laser in the Treatment of Patients with Rotator Cuff Tendinopathy: A Randomized Controlled Trial. Photomed Laser Surg. 2018;36(9):506-513.
- Dedes V, Stergioulas A, Kipreos G, Dede AM, Mitseas A, Panoutsopoulos GI. Effectiveness and Safety of Shockwave Therapy in Tendinopathies. Mater Sociomed. 2018;30(2):131-146.
- Kelle B, Kozanoglu E. Low-level laser and local corticosteroid injection in the treatment of subacromial impingement syndrome: a controlled clinical trial. Clin Rehabil. 2014;28(8):762-771.
- Anders JJ, Lanzafame RJ, Arany PR. Low-level light/laser therapy versus photobiomodulation therapy. Photomed Laser Surg. 2015;33(4):183-184.
- Karu TI. Low power laser therapy. In: Vo-Dinh T, ed. Biomedical Photonics Handbook. 2nd ed. Boca Raton,FL: CRC Press; 2003: 48-1-48-25.
- Hamblin MR, Demidova TN. Mechanisms of low level light therapy. Proc. of SPIE Photonics. 2006; 6140: 614001-01-12.
- da Silva, T.G., Ribeiro, R.S., Mencalha, A.L. et al. Photobiomodulation at molecular, cellular, and systemic levels. Lasers Med Sci 38, 136 (2023).
- Elsodany, A. M., Alayat, M. S. M., Ali, M. M. E., & Khaprani, H. M. (2018). Long-Term Effect of Pulsed Nd:YAG Laser in the Treatment of Patients with Rotator Cuff Tendinopathy: A Randomized Controlled Trial. Photomedicine and laser surgery, 36(9), 506–513.
- Page, M. J., Green, S., Mrocki, M. A., Surace, S. J., Deitch, J., McBain, B., Lyttle, N., & Buchbinder, R. (2016). Electrotherapy modalities for rotator cuff disease. The Cochrane database of systematic reviews, 2016(6), CD012225.
- Arroyo-Fernández R, Aceituno-Gómez J, Serrano-Muñoz D, Avendaño-Coy J. High-Intensity Laser Therapy for Musculoskeletal Disorders: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. J Clin Med. 2023;12(4):1479.
- Intelect RPW 2 User Manual. https://enovis-medtech.eu/media/storage.djoglobal.eu/en_US/Documents/Support_documents/IFU_13-28670_US_Rev_A_Intelect_RPW_2_DIGITAL_Final.pdf
- shockwave definition. Bing. Accessed December 18, 2023. https://www.bing.com/search?q=shockwave+definition&cvid=fc98a1ef85b74e16acacd38d178a34da&gs_lcrp=EgZjaHJvbWUqBggAEAAYQDIGCAAQABhAMgYIARBFGDkyBggCEAAYQDIGCAMQABhAMgYIBBAAGEAyBggFEAAYQDIGCAYQABhAMgYIBxAAGEAyBggIEAAYQDIICAkQ6QcY8gcyBwgKEEUY_FXSAQgyMTY5ajBqNKgCALACAA&FORM=ANAB01&PC=U531
- d’Agostino MC, Craig K, Tibalt E, Respizzi S. Shock wave as biological therapeutic tool: From mechanical stimulation to recovery and healing, through mechanotransduction. Int J Surg. 2015;24(Pt B):147-153.
- Fuchs J. Stable vs. Transient Cavitation. CTG Technical Blog. Published January 17, 2019. https://www.blackstone-ney.com/blog/stable-vs-transient-cavitation/
32 Enovis (2023). Post-Market Clinical Follow-Up Retrospective Study Report: LightForce® Therapy Lasers. Internal Enovis report. Unpublished.
